Mastering Mealtime in Dementia Care
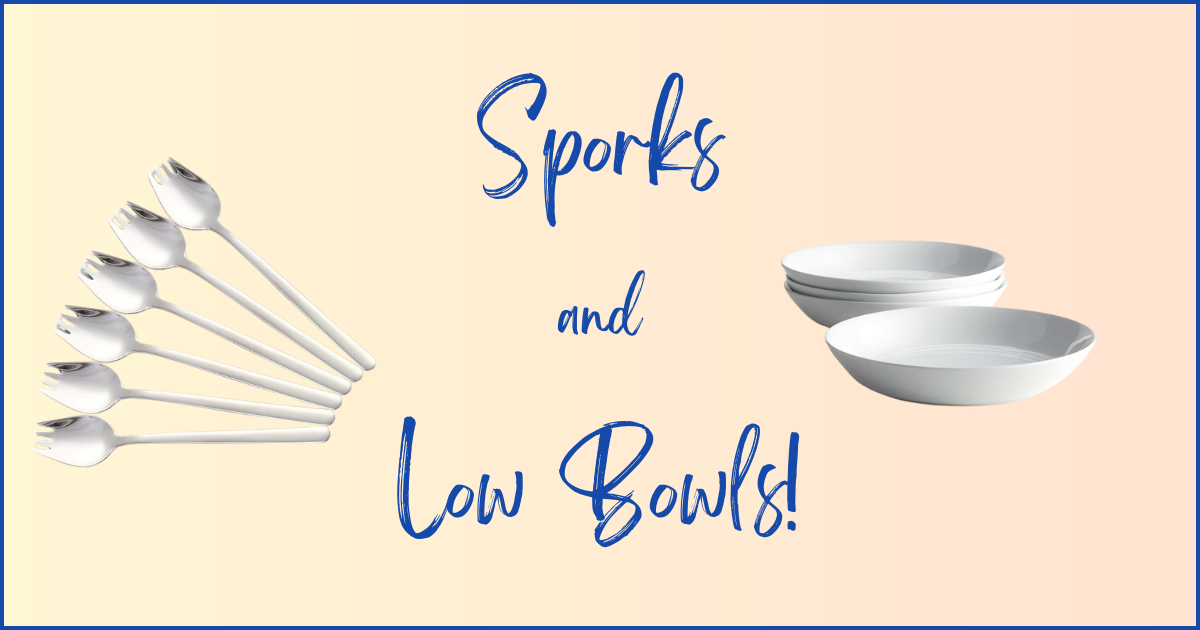
We wish we’d known about sporks and low bowls much earlier with our care receivers dining!
As caregivers for our loved ones with Alzheimer’s and other types of dementia, we’ve learned eating and drinking become significant challenges. Through our experiences, and what we’ve learned from support groups and others on their journeys, we’ve developed seven important tips to help you and your care receiver navigate dining.
Understanding Eating and Drinking Challenges in Dementia Care
One goal is to help our care receivers maintain their independence and dignity as long as possible. We’ll gradually transition from observing to prompting, to assisting, and finally to taking over the process completely. Their challenges can include difficulty preparing meals, using utensils, chewing and swallowing, recognizing hot and cold, maintaining both proper nutrition and hydration.
This area of our care requires continuous observation, adjustment, patience, creativity, and flexibility.
Here are the seven tips to help you and your care receiver navigate eating and drinking.
Tip 1: Observe Their Natural Eating Habits
Understanding your care receiver’s natural eating habits can reduce their confusion and help you provide better support throughout their journey.
Key points:
- Observe and record how they naturally eat and drink (e.g., time of day, order, how they cut their food, which hand they use for each utensil).
- What do they and don’t they like to eat and drink?
- Do they have preferences for food placement on their plate?
- Do they have sensitivities to heat and cold? Food textures?
- Continuously observe, adjust, and share with others who are helping your care receiver with their eating and drinking. Update as changes occur in their preferences and their abilities.
Sue’s Experience:
My dad was a man of habit around eating and drinking. He had a specific menu of what he wanted for breakfast. He wanted to drink, then eat. He didn’t like his food to touch on his plate. When he took a bite, he wanted a bit of each food on his plate on his fork or spoon. Through almost his entire dementia journey, he remembered this pattern. It was important for us to make sure anyone participating in his feeding clearly understood this. He did not naturally like to drink enough water. We put the total amount of water he needed to drink in a day out on the counter every day so we made sure he had enough to stay hydrated.
Tip 2: Utilize Pre-made Meals and Visual Cues
Early in their journey, pre-made meals can help maintain independence when supervision isn’t necessary.
Key points:
- Leave pre-made meals in easily accessible places (e.g., eye-level in the refrigerator).
- Use visual cues like notes on the refrigerator or preset table settings with a note where the plate will go that tells your care receiver where the meal is.
- Check to make sure they have actually eaten their food and finished what they had to drink so you know if they’re able to understand what to do.
- Be prepared to transition away from this strategy as their diagnosis progresses.
Nancy’s Experience:
For months this routine worked perfectly. When I was traveling, my husband would go to the freezer, get his dinner, and put it in the microwave. He was good to go… until one day he wasn’t. I was out of town and had a friend stop by around dinner time to make sure he had eaten his dinner. She called me and said: “When I got there, I asked him about his dinner. He said he didn’t have any food and didn’t know anything about fixing something to eat.
Tip 3: Pre-cut Food, Adjust Portions, Observe How They’re Able to Eat and Drink
As the diagnosis progresses, adjusting food presentation to simplify eating and portions to ensure they’re eating the amount healthy for them, becomes crucial.
Key points:
- Pre-cut food into manageable pieces.
- Consider converting sandwiches and other foods into finger foods.
- Be aware of changes in hand stability, grip strength, vision, and coordination.
- Test food temperature. They will lose the ability to judge if food is too hot or cold.
- Some people with dementia diagnoses lose regulation with their appetite. It’s important for us to observe how they’re eating and the portions they’re eating to make sure they’re getting the proper amount of food.
- With changes in attention span and loss of connection with appetite, you may adjust to having smaller meals throughout the day.
- Ice can become frightening. It makes noise, if your care receiver is lifting their glass to their mouth, it may shift, hit their mouth, and startle them.
- Look for signs of dysphasia (difficulty swallowing).
- Introduce non-breakable drinkware, consider tops or adult sippy cups.
Nancy’s Experience:
With both my husband and my father-in-law, a whole sandwich became too daunting. They would quit after a few bites. If we cut the sandwich into fourths, they would eat the whole thing.
Sue’s Experience:
My husband forgot which utensil to use and how to use them. For example, the knife and fork to cut the food and then take a bite, and when to use the utensil. I began putting food together that required one utensil at a time. For example, if we were having soup, I gave him a bowl with some soup and a spoon. There was no other food or silverware on the table. Other foods were cut to bite sized pieces. I would have either a fork or a spoon for him to use(oh, how I wish I’d known about sporks and low bowls!!!). He also lost the ability to discern hot and cold, so I was very careful to pre-taste everything.
Tip 4: Prepare for Messier Eating
Hand/eye coordination, depth perception, and/or hand stability of our care receiver may decline, making eating and drinking messier. If we get frustrated — which can easily happen — this is a good time for us to remind ourselves they would prefer to be able to eat and drink easily and on their own.
Key points:
- Consider using regular bibs, large disposable bibs or food catcher bibs.
- You can replace regular napkins with plastic backed disposable napkins to provide protection from spills.
- Place a towel on the chair to catch spills.
- Observe how your care receiver holds beverages and how they drink. They may forget how to raise their head to drink, or how to use a straw. There are adaptive cups for this.
- Keep a basket of cleaning supplies (e.g. paper towels, hand wipes, table wipes) handy for quick clean-ups.
- Give yourself and your care receiver lots of grace in the feeding and drinking process!
Tip 5: Simplify Eating Utensils and Tableware
Specialized and adaptive utensils and tableware make it easier for our care receiver to eat, to enjoy their food and beverages safely, and to maintain their independence longer. Fortunately there are a wide range of adaptive products available for the entire dining process.
Key points:
- Low bowls with a slight rim make it easier to push food onto utensils, reducing spills and helping get food onto the utensil.
- Sporks combine the functions of spoons and forks, so one utensil can be used. It is shaped like a spoon and has short tines of a fork.
- Grippy placemats keep plates from sliding.
- Adaptive utensils, beverage and tableware options provide better control.
Nancy’s Experience:
My husband was stabbing food with his spoon and unsuccessfully trying to scoop food with his fork. I thought “There has got to be a way to make this easier for him.” Then I thought of sporks. I initially thought of the old plastic sporks we used to get when we went to Kentucky Fried Chicken. Those were not going to work! After some research I found metal, tablespoon-sized sporks. They are fabulous. I really wish I’d thought of them earlier.
Tip 6: Monitor and Adjust Nutrition
This is an area where continuous monitoring and adjustment are important. There are a variety of reasons the weight of dementia patients changes. These include loss of appetite, forgetting to eat, not being hungry, not liking changes in the texture and/or taste of foods, developing different tastes in foods, changes in their sense of smell and taste, and changes in their vision.
Key points:
- Observe any changes in your care receiver’s relationship with food.
- Watch for unexplained weight loss or gain.
- Consult with doctors if you notice sudden changes.
- Be prepared to adjust calories and/or adjust meal frequency.
- If you move your care receiver to a memory care community, develop nutrition plans and weight monitoring processes and stay actively engaged with them.
Nancy’s Experience:
My husband was eating the same amount he always ate. One day we looked at him and I said, “Does anybody else think he’s suddenly lost a lot of weight?” We called the doctor, who came and conducted several tests including checking for any issue with his thyroid. The nurse explained there are brain chemistry changes with dementia that are unexplained, and can cause them to just lose weight. We shifted how much and how frequently he ate, and got him back to a healthy weight.
Tip 7: Gradually Take Over Feeding and Hydration
As the disease progresses, you’ll need to take a more active role in feeding and hydration.
Key points:
- Position yourself closer to them at mealtimes to make assistance easier.
- What begins as prompting them to eat or drink and gradually increases to handing them their utensils and/or putting food on their utensils, showing them their drinking glass becomes modifying their drinking glass to make it easier for them to use, to eventually fully feeding them and controlling their beverages.
Sue’s Experience:
I began moving closer to my care receiver. I was either diagonal to them or next to them. In the beginning, I was just having a conversation with them, observing them. This made it easier and less obvious as it became helpful to insert myself when my care receiver needed additional prompting and support.
Final Thoughts
Navigating eating and drinking challenges in Alzheimer’s and dementia care requires patience, continuous observation, flexibility and adaptability so we achieve our goal of maintaining their dignity and independence as long as possible, while ensuring their proper nutrition and hydration.
Key takeaways:
- Observe and respect your care receiver’s natural eating patterns.
- Gradually increase assistance as needed.
- Use adaptive tools like low bowls and sporks to promote independence.
- Monitor nutrition and hydration carefully, adjusting as necessary.
- Prepare for messier eating and give both yourself and your care receiver grace.
- Position yourself strategically to make assistance easier and less disruptive.
- Prioritizing hydration is just as important as nutrition.
- Record preferences so others can provide support.
If you have tips you think others would benefit from, please share them on our Facebook page or Instagram page.
We’re all on this journey together.
Connect with us and share your tips:
- Website: https://www.thecaregiversjourney.com
- Instagram: https://www.instagram.com/thecaregiversjourney/
- Facebook: https://www.facebook.com/TheCaregiversJourneys/
- Linkedin: https://www.linkedin.com/in/suearmstrongryan/, https://www.linkedin.com/in/nancytreaster/
- Email: [email protected], [email protected]
Additional Resources Mentioned:
Episode 13 — Incontinence Overnight here
These resources contain affiliate links so we may receive a small commission for purchases made at no additional cost to you.
Bibs here
Sporks here
Low bowls here
Grippy placemats here
Other great caregiver dining aid products here




Join the community