I wish I’d realized I didn’t have to complete grooming tasks at one time!
As caregivers for our loved ones with Alzheimer’s and other types of dementia, we’ve learned that shaving, trimming nails, brushing teeth and trimming hair — what we’re calling personal care — can become challenging. These challenges often arise around the same time as bathing and dressing difficulties.
How we provide support for our loved one will vary based on whether they stay at home during their journey or move into a care community. Not surprisingly, personal care is an area where many tips can be provided!
Through our experiences, what we’ve learned from support groups, and others on their journeys, we’ve developed four initial areas of tips to help you and your care receiver with their personal care.
Understanding Personal Care Challenges in Dementia Care
Before we share our tips, it’s helpful to understand what to expect.
For all personal care areas, it’s helpful to talk with our care receiver early in their journey to learn about their current choices. Have conversations with them about what is most important to them, work together to simplify their personal care choices, and ask them about any issues they deal with that you may not be aware of. Begin supporting them while they can still guide you, so you learn how to care for them as they become more challenged caring for themselves.
These prepare them, you, and other caregivers who either support them at home or in a care community, so everyone is prepared to provide the best care.
Nancy’s Experience:
“I really wish I’d known this tip earlier around personal care. Sue taught me that it’s okay to just do part of it, you don’t have to get it all done at one time! This was truly transformational. I had no idea, and it’s brilliant.” (More about this tip below.)
Sue’s Experience:
I learned to meet my care receiver exactly where they are in the moment, moment by moment. I let go of expectations of what we had done in the past and embrace what we have access to in this moment we have.
Here are four tips to help you navigate personal care challenges:
Tip 1: Mastering the Art of Shaving
As the journey progresses, shaving becomes a task you need to assist with and gradually take over entirely.
Key points:
- Transition to an electric razor as early as possible. It’s safer for your loved one, easier for you to use and, if you move your loved one into a memory care community, they won’t be allowed to have a manual razor.
- Electric razor blades get dull! Keep an extra set on hand and the instant the blade pulls your loved one’s hair, change them.
- Begin your support by prompting and supervising, gradually inserting yourself into the process.
- For men’s facial hair, talk with your loved one about shaving it off while they’re still able to help. If not, seek advice from either a friend or barber if you’re unfamiliar with mustache or beard maintenance.
- Try shaving when your care receiver is calm, possibly after meals or during naps.
- Aim to shave men’s facial hair at least every other day to prevent discomfort from longer hair.
- For women, transition to electric razors for safety. Women also tend to become comfortable with letting their body hair grow. Experiment to see if your female care receiver is ok without shaving.
Nancy’s Experience:
Soon after my husband was diagnosed, for some reason I knew we needed to transition to an electric razor. I had my children give him one for Christmas. He looked at it kind of funny, unexpectedly, because he didn’t use an electric razor. It was easy for me, over the next few weeks, to get him to use it by saying “Let’s get the electric razor the kids gave you for Christmas.”
Tip 2: Nail Care Techniques
Important note: We are not doctors and we are not offering medical advice. If your loved one is diabetic, please make sure you know if it is prescribed for their toenails to be trimmed by a podiatrist. Some people with diabetes have poor circulation and nerve damage in their feet. This makes them highly susceptible to infections from even small cuts or injuries that can happen during toenail trimming — especially if they are resistant to your support.
While trimming fingernails and toenails can be challenging, it is important for comfort, hygiene, and safety. If you’re not familiar with trimming the finger and/or toenails of someone else, as soon as your care receiver is diagnosed, go to a nail salon and ask them to teach you how.
Sue’s Experience:
I learned two big tips during one of my first caregiving journeys:
Practice with my care receiver early in their diagnosis when they could share what they liked or didn’t like (I also brought this into many areas of caregiving support and my other caregiving journeys.).
I had never trimmed anyone else’s nails and I had no idea how to when I was facing them. I went to a professional and had them teach me how to give a basic manicure and pedicure. I practiced with a few very supportive friends to get used to it!
Key points:
- Start by observing their natural nail care routine.
- Gradually insert yourself into their process.
- Consider professional nail care services if you’re not comfortable.
- Use sharp implements for easier trimming.
- If your hands are naturally cold, wear thin cotton gloves.
- Use warm water to soak their hands and feet.
- For ticklish feet, use firm pressure or a towel to reduce sensitivity.
- Focus on safety and function rather than fashion and style.
- Use wooden manicure sticks to clean under their nails.
Sue’s Experience:
As his diagnosis progressed, my husband was good for about one nail, then he would just start pulling it away. I would simply trim one nail at a time and not even try to do two at once.
I had great success trimming all his nails when he was asleep — either his afternoon nap, or while he was sleeping at night.
My dad’s feet were incredibly ticklish. I used the cotton gloves to make sure my hands weren’t cold, put a towel around his foot and used firm pressure so I wasn’t tickling him. I alternated his feet multiple times during the pedicure, so there wasn’t continuous focus on one foot.
Tip 3: Dental Hygiene Strategies
Maintaining good oral health is crucial, however, this can become a very challenging part of hygiene.
Key points:
- As early in their diagnosis as possible, get a thorough dental examination. If there is any dental work that’s important to be completed, do it while they still understand and can participate.
- As your care receiver’s diagnosis advances, almost every part of the dental experience becomes more difficult for you, your care receiver, and the dentist, beginning with struggling to get in the car.
- Many parts of their experience become more fearful for your care receiver including struggling to get in the dentist chair.
- Consider transitioning to a dentist specializing in disabilities.
- Some cities have mobile dentists. Some only go to care communities, some make house calls. If your care receiver is at home, reach out to care communities to ask if they have a mobile dentist for their contact information.
- If possible increase dental visits to every three months.
- Start by reminding your care receiver and supervising their tooth brushing.
- Gradually take over the process — for example, begin by handing them their toothbrush, transition to handing them their toothbrush with toothpaste on it, then transition to beginning to brush their teeth.
- Use a soft-bristled toothbrush and less toothpaste to prevent swallowing.
- Consider using disposable oral swabs with mouthwash for additional cleaning.
- Be patient through non-compliant phases; they often pass.
Nancy’s Experience:
There was a point for around a year and a half where, if we just got the toothbrush in my husband’s mouth at one time during the day, we thought that was a win. Now we’re back to the other side where we are able to brush his teeth three times a day.
Sue’s Experience:
Unlike Nancy’s experience, my husband became less and less compliant as his diagnosis progressed. He didn’t get to a point where he became compliant again. We used oral swabs in his mouth when he was asleep.
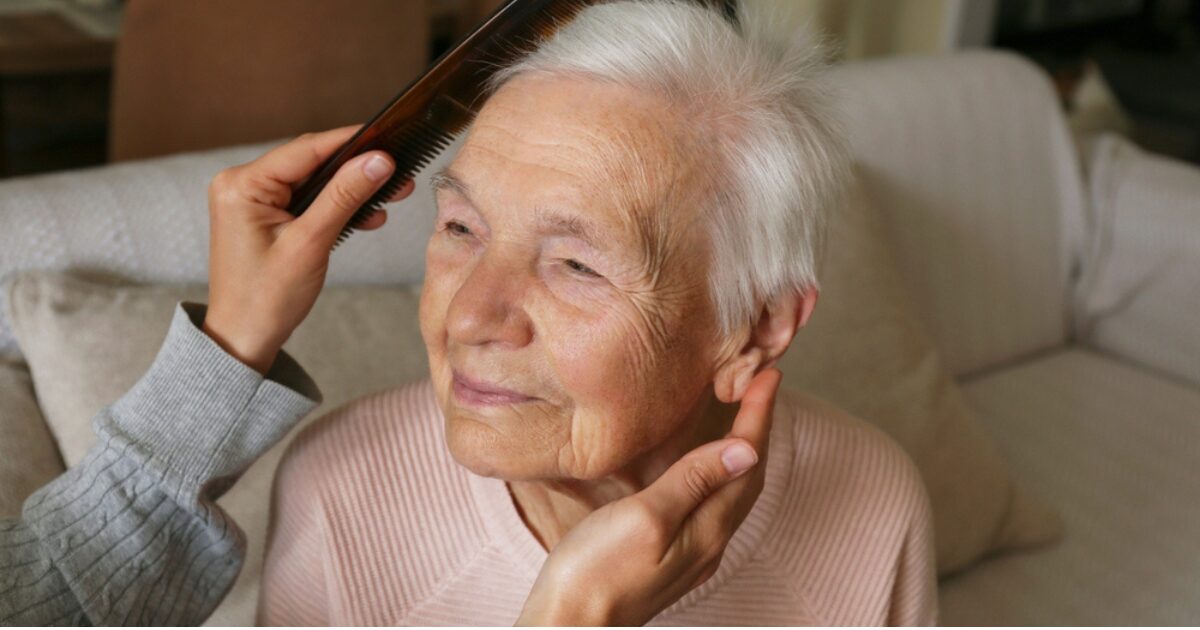
Tip 4: Hair Care and Trimming
Hair care involves the hair on their head, their eyebrows, nose, and ears.
Key points:
- Take photos of the hair style your loved one has.
- Talk with them early in their diagnosis about what they like/don’t like about their current hairstyle.
- If they color their hair, talk about keeping it colored or letting it become their natural color.
- There are hair stylists who will come to your home instead of you having to go into a salon. Most care communities offer services of both hair and nail stylists.
- Consider transitioning to easier-to-manage hairstyles.
- Learn basic haircutting techniques or ask their stylist to teach you.
- Be aware of cowlicks and natural hair patterns when cutting.
- For women, longer hair in a soft bun might be easier than short styles.
- Personal care trimmers are very helpful for both men and women for eyebrows, hair in the ears and nose. If your care receiver isn’t used to these, it’s helpful to get them used to the sound and vibration early in their journey so you’re not introducing anything new for them later on.
Sue’s Experience:
With my Dad, his stylist began coming to their home. My Dad wasn’t comfortable with strangers touching him, so his familiarity with her made it easy for him to have his hair cut.
With my husband, I had begun cutting his hair while he was at home and he was fine with that. When I moved him into memory care, I would take him to the stylist at the care facility and that was fine until he forgot how to sit in the chair. No matter what we did he couldn’t get in the chair. The stylist couldn’t use a chair that couldn’t be adjusted, so I began cutting Jack’s hair again. When he began being resistant, I just cut whatever part I could cut until he was done. I would go back later and begin again. If he remained resistant, I’d just cut his hair when he was sleeping.
Final Thoughts:
Navigating personal care challenges in Alzheimer’s and dementia care requires patience, creativity, and flexibility. You don’t have to complete all tasks at once — or perfectly — every time.
Key takeaways:
- Transition to safer tools like electric razors and trimmers.
- Gradually increase your involvement in the grooming process.
- Be patient through non-compliant phases; they often pass.
- Consider grooming during calm times, like after meals or during naps.
- Focus on safety and comfort rather than perfect appearance.
- Give yourself and your care receiver grace as you navigate these changes.
This is an especially important area to remember you’re not alone on this journey. If you have tips you think others would benefit from, please share them on our Facebook page or Instagram page.
We’re all on this journey together.
Additional Resources Mentioned:
These resources contain affiliate links so we may receive a small commission for purchases made at no additional cost to you.
Electric razor
Oral swabs here
Super soft toothbrush here
Fresh Breath mouthwash here
Electric hair trimmers here




Join the community